Amidst the multifaceted domain of urology, diagnostic tests serve as vital tools for unraveling the enigmatic nature of urological conditions. These tests, including urodynamics tests and various other urology diagnostic tests, bear immense significance in identifying and evaluating diverse urological disorders. This blog aims to immerse readers in the world of urology, offering a comprehensive exploration of the most common tests employed by male urologists to diagnose and manage these conditions. Through the prism of scientific rigor, we shall shed light on the intricacies of urinalysis, blood tests, imaging studies, cystoscopy, prostate biopsies, ureteroscopy, and uroflowmetry, unveiling their roles in the intricate tapestry of urological diagnostics. Delve into this captivating journey, as we demystify the complexities of these tests.
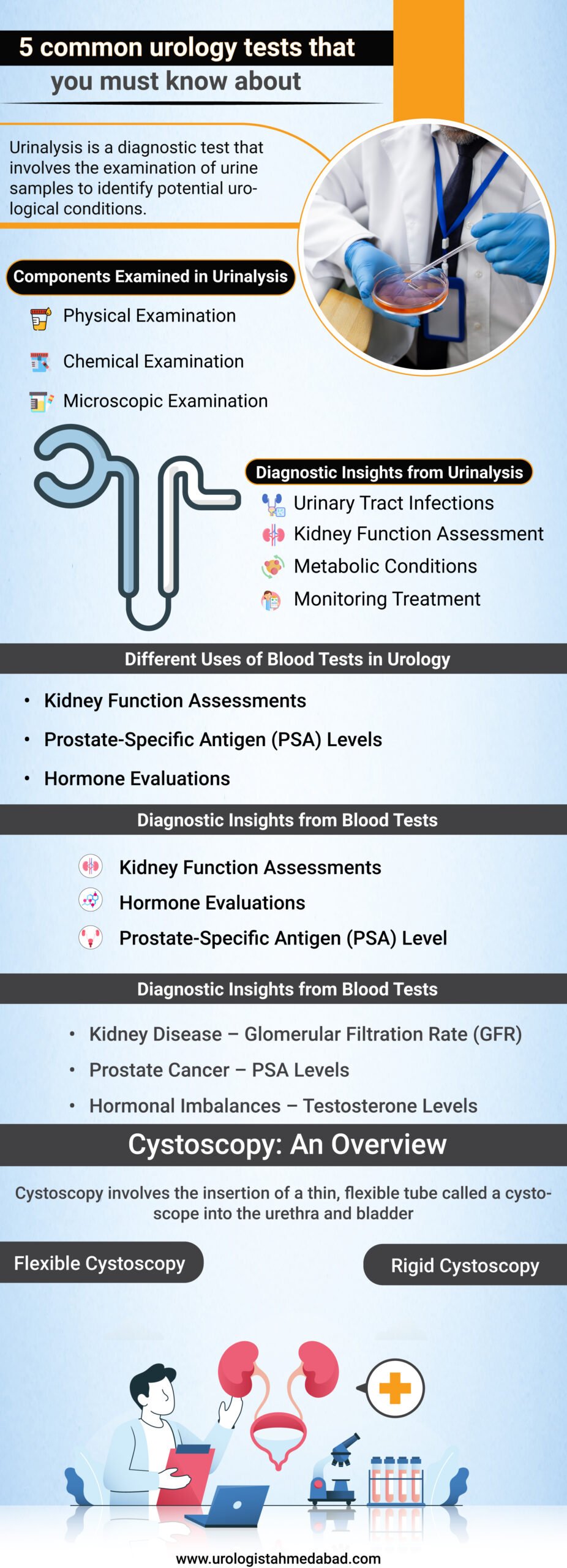
Table of Contents
1. Understanding Urinalysis
Urinalysis is a diagnostic test that involves the examination of urine samples to identify potential urological conditions. Urinalysis plays a crucial role in detecting abnormalities within the urinary system, aiding in the diagnosis and management of urological disorders.
Components Examined in Urinalysis
- Physical Examination –
- Color: The color of urine can indicate hydration levels or the presence of certain conditions.
- Clarity: The clarity of urine can provide insights into the presence of substances such as bacteria or mucus.
- Odor: Certain odors may suggest infections or metabolic disorders.
- Chemical Examination –
- pH Levels: The acidity or alkalinity of urine can offer insights into various conditions.
- Specific Gravity: This measures the concentration of urine and can indicate hydration status or kidney function.
- Protein: The presence of protein may indicate kidney damage or other renal disorders.
- Glucose: Elevated glucose levels may suggest diabetes or other metabolic conditions.
- Ketones: The presence of ketones can indicate metabolic disorders or certain dietary conditions.
- Microscopic Examination –
- Red Blood Cells (RBCs): Elevated RBCs may suggest urinary tract infections, kidney stones, or other disorders.
- White Blood Cells (WBCs): Increased WBCs can be indicative of urinary tract infections or inflammation.
- Bacteria: The presence of bacteria may indicate urinary tract infections.
- Crystals: Certain types of crystals may be associated with kidney stones or metabolic conditions.
Diagnostic Insights from Urinalysis
- Urinary Tract Infections: Urinalysis helps detect the presence of bacteria, WBCs, or abnormal pH levels, aiding in the diagnosis of UTIs.
- Kidney Function Assessment: Abnormal protein levels, RBCs, or specific gravity can provide insights into kidney function and potential disorders.
- Metabolic Conditions: Detection of glucose, ketones, or other abnormal components assists in identifying metabolic disorders.
- Monitoring Treatment: Regular urinalysis can help evaluate the effectiveness of urological treatments and track progress.
2. Different Uses of Blood Tests in Urology
- Kidney Function Assessments
- Definition: Blood tests are employed to evaluate kidney function by measuring certain markers within the blood.
- Significance: These tests aid in diagnosing and monitoring kidney diseases and disorders, providing valuable insights into renal health.
- Prostate-Specific Antigen (PSA) Levels
- Definition: PSA is a protein produced by the prostate gland, and blood tests measure its levels within the bloodstream.
- Significance: PSA tests are used primarily to screen for prostate cancer, helping detect and monitor the progression of the disease.
- Hormone Evaluations
- Definition: Blood tests analyze hormone levels to assess hormonal imbalances or abnormalities.
- Significance: Hormone evaluations play a pivotal role in diagnosing conditions related to the male urological system, such as testosterone deficiencies or hormonal disorders.
Diagnostic Insights from Blood Tests
- Kidney Disease – Glomerular Filtration Rate (GFR): GFR calculations estimate the efficiency of kidney function, aiding in the diagnosis and staging of kidney disease. – Creatinine Levels: Elevated creatinine levels suggest impaired kidney function, indicating potential renal disorders.
- Prostate Cancer – PSA Levels: Elevated PSA levels may indicate the presence of prostate cancer, prompting further diagnostic investigations. – PSA Velocity: Changes in PSA levels over time can provide insights into the aggressiveness of prostate cancer.
- Hormonal Imbalances – Testosterone Levels: Blood tests measure testosterone levels, helping identify deficiencies or abnormalities that may impact urological health. – Other Hormones: Evaluating additional hormones, such as luteinizing hormone (LH) or follicle-stimulating hormone (FSH), aids in diagnosing hormonal disorders.
Monitoring Treatment and Disease Progression
- Blood tests are employed to monitor the effectiveness of urological treatments, assess disease progression, and make informed adjustments to the management plan.
3. What are the different imaging modalities and how do they aid in the detection of urological abnormalities?
- Ultrasound
- Definition: Ultrasound employs high-frequency sound waves to produce real-time images of the urinary system.
- Significance: This non-invasive imaging technique is used to assess the kidneys, bladder, and other structures, aiding in the detection of abnormalities and guiding urological diagnoses. X-ray
- X-ray
- Definition: X-ray imaging utilizes electromagnetic radiation to create images of the urinary system.
- Significance: X-rays can reveal the presence of kidney stones, identify structural abnormalities, and assist in the diagnosis of conditions such as urinary tract infections or blockages.
- Computed Tomography (CT) Scan
- Definition: CT scans utilize X-ray technology and computer processing to generate cross-sectional images of the urinary system.
- Significance: CT scans provide detailed and three-dimensional images, allowing for the detection and characterization of kidney stones, tumors, and other urological abnormalities with exceptional precision.
- Magnetic Resonance Imaging (MRI)
- Definition: MRI employs a powerful magnetic field and radio waves to produce detailed images of the urinary system.
- Significance: MRI offers exceptional soft tissue visualization, enabling the identification and evaluation of urological conditions such as tumors, structural abnormalities, and inflammation.
Diagnostic Insights from Imaging Techniques
- Kidney Stones – Imaging techniques facilitate the detection, localization, and evaluation of kidney stones, aiding in the determination of appropriate treatment options.
- Tumors and Cancer – Imaging modalities play a crucial role in the detection, staging, and monitoring of urological tumors, including kidney, bladder, or prostate cancer.
- Structural Abnormalities – Detailed imaging allows for the identification of structural issues within the urinary system, such as urinary tract obstruction or congenital abnormalities.
Guiding Treatment and Intervention
- Imaging techniques guide surgical interventions, help monitor treatment response, and enable the precise placement of urological devices or interventions.
4. Cystoscopy: An Overview
Cystoscopy involves the insertion of a thin, flexible tube called a cystoscope into the urethra and bladder. This procedure allows urologists to directly examine the urinary tract, providing valuable insights into urological conditions.
Diagnostic Insights from Cystoscopy
- Urinary Blockages – Visual Evaluation: Cystoscopy enables the direct visualization of the urethra and bladder, allowing the identification of obstructions, strictures, or other urinary blockages. – Treatment Planning: The visualization of blockages aids in planning appropriate treatments, such as urethral dilation or the placement of stents.
- Bladder Infections – Identification of Inflammation: Cystoscopy allows urologists to observe signs of bladder inflammation, such as redness, swelling, or ulcerations, suggesting the presence of infections. – Sample Collection: During cystoscopy, tissue samples or urine specimens can be obtained for laboratory analysis, aiding in the diagnosis of infections.
- Bladder Cancer – Visual Inspection: Cystoscopy provides direct visualization of the bladder lining, allowing the identification of abnormal growths, tumors, or suspicious lesions. – Biopsy: During cystoscopy, tissue samples can be collected through the cystoscope for further evaluation, aiding in the diagnosis and staging of bladder cancer.
Types of Cystoscopy
- Flexible Cystoscopy – Description: Flexible cystoscopy involves the use of a thin, flexible cystoscope, which provides excellent maneuverability and allows for a detailed examination of the urinary tract. – Advantages: It is less invasive, typically performed under local anesthesia, and can be conducted in an office or outpatient setting.
- Rigid Cystoscopy – Description: Rigid cystoscopy involves the use of a rigid cystoscope, which provides a larger working channel and allows for interventions, such as stone removal or tissue cauterization. – Advantages: It offers greater control and accessibility for surgical procedures, often performed under general or regional anesthesia in a hospital setting.
Patient Experience and Potential Risks
- Patient Comfort: Cystoscopy may cause mild discomfort, which can be managed through local anesthesia or, in some cases, sedation.
- Potential Risks: Although rare, potential risks include urinary tract infection, bleeding, perforation, or allergic reactions to anesthesia or contrast agents.
5. What is Urodynamic Testing?
Urodynamic testing refers to a series of diagnostic procedures that assess the function and performance of the lower urinary tract. This specialized testing enables the evaluation of bladder storage, emptying, and coordination, assisting in the diagnosis and management of urological disorders.
Diagnostic Insights from Urodynamic Testing
- Bladder Storage Function – Cystometry: This test measures bladder pressure and capacity during filling, aiding in the evaluation of conditions like overactive bladder or bladder instability. – Pressure-Flow Study: It assesses bladder pressure and urine flow rate during voiding, helping identify bladder outlet obstruction or other voiding dysfunctions.
- Bladder Emptying Function – Uroflowmetry: Urodynamic testing includes measuring the urine flow rate during voiding, and assisting in the assessment of bladder emptying and potential obstructions. – Post-void Residual Measurement: This evaluates the amount of urine left in the bladder after voiding, providing insights into incomplete emptying or urinary retention.
- Bladder Coordination and Control – Electromyography (EMG): EMG measures the electrical activity of the muscles involved in bladder control, aiding in the evaluation of conditions like neurogenic bladder or detrusor sphincter dyssynergia. – Leak Point Pressure Measurement: This assesses the pressure at which urine leakage occurs, assisting in the diagnosis and management of stress urinary incontinence.
Types of Urodynamic Testing
- Video Urodynamics – Description: Video Urodynamics combines fluoroscopy or ultrasound imaging with pressure measurements, providing a visual and dynamic assessment of bladder function. – Advantages: It offers real-time visualization, allowing for the identification of anatomical abnormalities, bladder contractions, or vesicoureteral reflux.
- Ambulatory Urodynamic Monitoring – Description: Ambulatory monitoring involves the use of portable devices to assess bladder function during daily activities, providing a more comprehensive evaluation. – Advantages: It allows for assessment in a natural setting, capturing information during different activities and positions, and aiding in the diagnosis of complex cases.
Patient Experience and Potential Risks
- Patient Preparation: Urodynamic testing may involve the insertion of catheters, filling the bladder, or performing specific maneuvers, necessitating detailed instructions and pre-test preparations.
- Potential Risks: While urodynamic testing is generally safe, potential risks include urinary tract infection, discomfort during catheter insertion or bladder filling, and transient blood in the urine.
Conclusion
The world of urology diagnostic tests encompasses a diverse array of techniques that play a pivotal role in the identification, evaluation, and management of urological conditions. From urinalysis and blood tests, providing insights into kidney function, hormonal imbalances, and prostate cancer, to imaging modalities such as ultrasound, X-ray, CT scans, and MRI, enabling detailed visualization of the urinary system, each test offers valuable information for accurate diagnoses. Furthermore, cystoscopy provides direct visualization of the urinary tract, aiding in the detection of urinary blockages, infections, and bladder cancer. Lastly, urodynamic testing offers comprehensive assessments of bladder function, highlighting storage, emptying, and coordination aspects. Together, these diagnostic tools enhance the diagnostic capabilities of urologists, ensuring comprehensive patient care within the field of urology. For more information or to schedule an appointment, reach out to Dr. Dushyant Pawar, a trusted urologist specializing in urology tests and diagnostics, committed to providing personalized care and accurate diagnoses to patients.



