Urine, a vital indicator of our body’s health, is typically clear with a faint yellow hue. However, when urine appears cloudy or contains visible particles, it signals the presence of sediments in urine Understanding the causes of sediments in urine includes various types like amorphous sediment and different presentations such as cloudy urine with white sediment, microscopic urine sediment, more, is crucial for effective diagnosis and treatment.
Table of Contents
What causes Sediments in Urine?
Sediments in urine often raise concerns about underlying health issues. Below is a closer look at its potential causes.
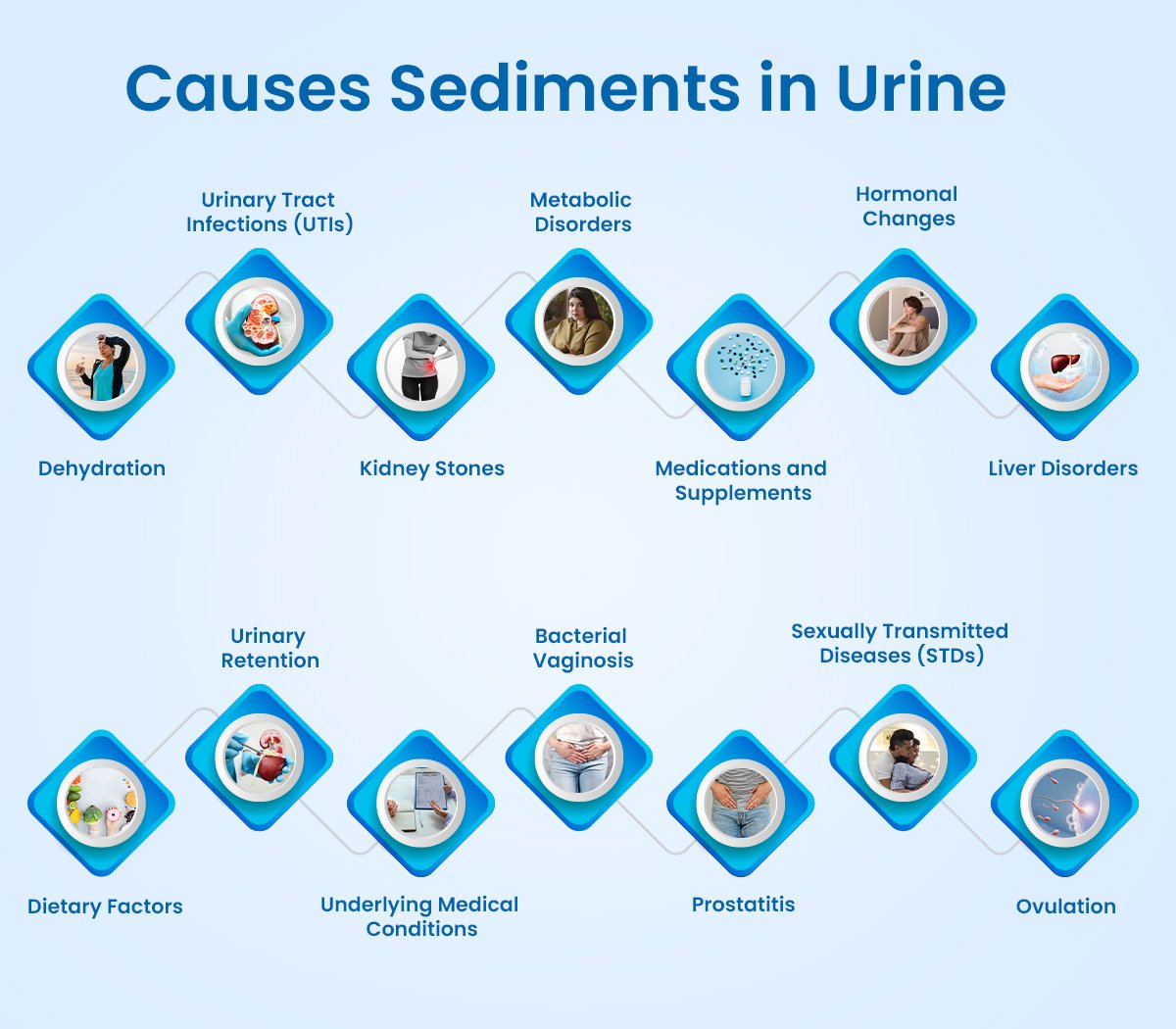
- Dehydration: Inadequate fluid intake can lead to concentrated urine, increasing the likelihood of sediment formation. When the body lacks sufficient hydration, urine becomes more concentrated, allowing substances like salts and minerals to precipitate and form sediment. Symptoms of dehydration include decreased urine output, darker urine color, and cloudy urine, all of which may indicate the presence of sediments in urine.
- Urinary Tract Infections (UTIs): UTIs are among the most common causes of sediments in urine. Bacterial infection of the urinary tract can lead to inflammation and the presence of pus or white blood cells in the urine, resulting in cloudy appearance and sedimentation. Symptoms often include frequent urination, a burning sensation during urination, and cloudy or foul-smelling urine.
- Kidney Stones: Hardened mineral deposits, known as kidney stones, can form in the kidneys or bladder and cause sediments in urine. These stones may consist of various substances such as calcium, oxalate, uric acid, or cystine. When these minerals crystallize and aggregate, they can create visible sediments in urine, along with symptoms like severe abdominal or flank pain, blood in urine, and difficulty urinating.
- Metabolic Disorders: Certain metabolic conditions, such as hypercalciuria (excessive calcium in urine) or hyperuricosuria (high uric acid levels in urine), can predispose individuals to urine sediment formation. Metabolic imbalances can lead to the excessive excretion of minerals or substances in urine, increasing the likelihood of sedimentation.
- Medications and Supplements: Some medications or dietary supplements can influence urine composition and promote sedimentation. For example, antacids containing calcium carbonate can raise urine pH, facilitating the formation of calcium phosphate crystals. Additionally, certain antibiotics or diuretics may alter urine characteristics and contribute to sediment formation.
- Hormonal Changes: Hormonal fluctuations, such as those occurring during pregnancy or ovulation, can affect urine composition and promote sedimentation. Pregnant individuals may experience changes in urinary pH or increased excretion of certain substances, leading to sediment formation. Similarly, hormonal fluctuations during the menstrual cycle can influence urine appearance and sedimentation.
- Liver Disorders: Liver conditions, such as hepatitis or cirrhosis, can impact urine composition and promote sediment formation. Liver dysfunction may lead to alterations in bilirubin metabolism, resulting in the presence of bilirubin crystals or pigment in urine. Additionally, liver disease can affect the body’s ability to metabolise certain substances, leading to changes in urine characteristics.
- Dietary Factors: Dietary habits can influence urine composition and promote sedimentation. Consuming foods high in oxalate, purines, or calcium can increase the risk of crystal formation in urine, contributing to sedimentation. Similarly, excessive intake of protein or sodium can impact urine pH and mineral excretion, leading to sediments in urine.
- Urinary Retention: Incomplete bladder emptying, often due to conditions like urinary obstruction or neurological disorders, can cause accumulation of sediments in urine. When urine remains stagnant in the bladder for extended periods, minerals and other substances have more time to precipitate and form sediments in urine.
- Underlying Medical Conditions: Various underlying health conditions, such as urinary tract abnormalities, systemic diseases (e.g., diabetes mellitus), or autoimmune disorders, can contribute to sediments in urine. These conditions may alter urine composition, impair kidney function, or promote inflammation, leading to sediment formation as a secondary effect.
- Bacterial Vaginosis: Inflammation of the vagina caused by an imbalance of bacteria is known as bacterial vaginosis. It can lead to changes in urine appearance, including the presence of sediments in urine, along with symptoms like foul-smelling urine and a burning sensation while urinating.
- Prostatitis: Inflamed prostate glands in men can lead to cloudy sediments in urine, often accompanied by painful urination and frequent urination.
- Sexually Transmitted Diseases (STDs): STDs such as chlamydia, gonorrhoea, and trichomoniasis can cause changes in urine appearance, including sediments in urine. Symptoms may also include pelvic pain, a burning sensation while urinating, and discharge in the urine.
- Ovulation: Hormonal changes during ovulation can lead to increased mucus production, which may resemble sediments in urine. This may be accompanied by other symptoms related to ovulation.
Different Types of Sediments in Urine:
- Crystals: Crystals in urine are formed when certain substances, such as calcium oxalate, uric acid, or struvite, precipitate out of solution. These crystals can vary in shape and size and may indicate conditions like kidney stones or metabolic disorders.
- Red Blood Cells (RBCs): The presence of red blood cells in urine, known as hematuria, can give urine a reddish or pinkish appearance. Hematuria may result from various conditions, including urinary tract infections, kidney stones, or kidney diseases, and lead to sediments in urine.
- White Blood Cells (WBCs): White blood cells in urine, known as pyuria, are indicative of inflammation or infection in the urinary tract. Elevated levels of WBCs may suggest conditions like urinary tract infections or interstitial cystitis and appear like sediments in urine.
- Epithelial Cells: Epithelial cells are shed from the lining of the urinary tract and may be present as sediments in urine. The presence of epithelial cells may indicate irritation, inflammation, or damage to the urinary tract.
- Bacteria: Bacteria in urine sediment may indicate urinary tract infections (UTIs). The identification of specific bacteria in urine can help diagnose the type of infection and guide appropriate treatment.
- Cast: Urinary casts are cylindrical structures formed from protein or cellular debris that become moulded within the kidney tubules. Different types of casts, such as hyaline casts, granular casts, or cellular casts, may indicate various kidney diseases or conditions.
- Crystalline Material: In addition to crystals formed from specific substances, urine sediment may contain amorphous crystalline material with no distinct shape. This material may include amorphous urates, phosphates, or calcium carbonate.
- Fat Globules: Fat globules may be present in urine sediment in conditions like nephrotic syndrome, where there is excessive protein loss in urine. The presence of fat globules may indicate lipiduria, a condition characterised by the presence of lipids in urine.
- Mucus: Mucus may be present in urine sediment, especially in individuals with urinary tract infections or inflammation. Excessive mucus production may indicate conditions like bacterial vaginosis or urethritis.
- Fungi: In cases of fungal infections of the urinary tract, fungal elements may be observed in urine sediment. Identification of fungal elements can aid in diagnosing fungal urinary tract infections and guiding appropriate treatment.
- Amorphous Sediment: Amorphous sediment refers to non-crystalline particles suspended in urine that lack a distinct shape or structure. These particles are often composed of amorphous phosphates, urates, or other substances. Amorphous sediment may appear as cloudy or hazy deposits in urine and is commonly observed during routine urine analysis. It can provide valuable insights into urinary tract health and metabolic status. Excessive or persistent amorphous sedimentation may indicate underlying conditions such as urinary tract infections, metabolic disorders, or dietary factors. Monitoring changes in amorphous sediment composition can aid in the diagnosis and management of urinary tract conditions.
How are Sediments in Urine Examined and Analysed?
Sediments in urine are examined through a process called urinary sediment analysis, which involves several steps:
- Sample Collection: A urine sample is collected from the patient using a clean, sterile container. The sample should ideally be a midstream catch to minimise contamination from the urethra.
- Sample Preparation: The urine sample is centrifuged to separate the solid components (sediment) from the liquid (urine). Centrifugation allows the sediment particles to settle at the bottom of the tube, forming a pellet.
- Microscopic Examination: A small amount of the sediment is transferred onto a glass slide and covered with a coverslip. The slide is then placed under a microscope, typically at low and high magnifications, to examine the sediment particles.
- Identification of Components: The examiner systematically scans the sediment under the microscope to identify various components, including red blood cells, white blood cells, epithelial cells, crystals, casts, bacteria, fungi, and other particles.
- Quantification: The number of each type of particle is quantified to assess their abundance in the urine sample. This quantitative analysis helps in determining the significance of the findings and may aid in diagnosing underlying conditions.
- Reporting Findings: The findings of the urinary sediment analysis are documented in a report, which includes details such as the types and quantities of sediment components observed, as well as any abnormal or clinically significant findings.
- Interpretation: The results of the urinary sediment analysis are interpreted in conjunction with the patient’s clinical history, symptoms, and other laboratory tests. This comprehensive approach helps in making accurate diagnoses and guiding appropriate treatment decisions.
- Follow-up: Depending on the findings of the urinary sediment analysis, further diagnostic tests or interventions may be recommended. Additionally, periodic monitoring of urinary sediment may be required to assess treatment response or disease progression.
Treatment for sediments in urine
The treatment for sediments in urine depends on the underlying cause and may include:
- Hydration: Increasing fluid intake helps dilute urine and prevents sediment formation, particularly in cases of dehydration.
- Antibiotics: If a urinary tract infection is identified as the cause, antibiotics are prescribed to eradicate the infection and clear the sediment in urine.
- Medications: Depending on the specific condition, medications may be prescribed to manage underlying issues such as kidney stones, metabolic disorders, or urinary tract abnormalities.
- Dietary Changes: Adjusting diet to reduce intake of substances that contribute to sediment formation, such as purines, oxalates, or sodium, may be recommended.
- Lifestyle Modifications: Making lifestyle changes, such as maintaining proper hygiene, avoiding prolonged urinary retention, and practising safe sex to prevent sexually transmitted infections, can help manage sediment formation.
- Surgical Intervention: In cases of large kidney stones or other structural abnormalities causing sedimentation, surgical procedures may be necessary to remove obstructions or correct underlying issues.
- Management of Underlying Conditions: Treating underlying medical conditions, such as diabetes, liver disease, or hormonal imbalances, can help reduce sediment formation in urine.
- Follow-up Care: Regular monitoring and follow-up appointments with healthcare providers are essential to assess treatment effectiveness, prevent recurrence, and monitor overall urinary tract health.
In Conclusion
In conclusion, microscopic analysis of sediments in urine is crucial for diagnosing urinary tract disorders, including infections and kidney stones. By meticulously examining sediment components, healthcare providers gain valuable insights into patients’ conditions, enabling personalised treatment strategies. Dr. Dushyant Pawar’s pioneering contributions have significantly advanced urinary sediment analysis, emphasizing its importance in modern healthcare. Embracing advancements in technology and research ensures continued enhancement of diagnostic accuracy, promoting urinary tract health and patient well-being.



