Urinary hesitancy, a prevalent concern cutting across age groups, unveils itself as more than a mere inconvenience—it often signals underlying health intricacies. In this exhaustive exploration, we embark on a deeper dive into the causes of urinary hesitancy, understanding the multifaceted tapestry that weaves this complex condition into the fabric of our health.
Table of Contents
What is Urinary Hesitancy?
Urinary hesitancy, characterized by difficulties initiating or maintaining a urine stream, is a condition that transcends age. While often associated with older men, the intricacies of this phenomenon require exploration into diverse factors contributing to its occurrence.
Urinary Hesitancy Causes: An In-Depth Look
1. Enlarged Prostate: A Common Culprit
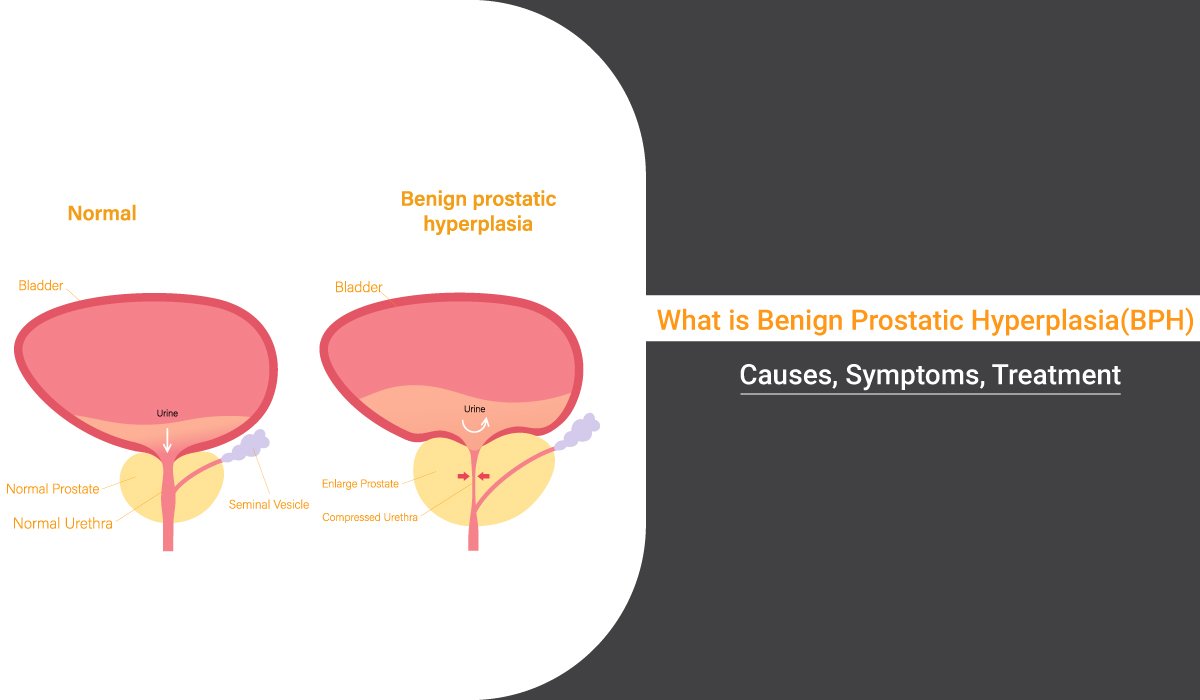
- Benign Prostatic Hyperplasia (BPH): Prevalent in men, BPH disrupts urine flow as the prostate enlarges, exerting pressure on the urethra.
- Age-Related Impact: While common in older men, BPH can affect individuals of various age groups.
2. Nervous System Disorders and Nerve Damage
- Accidents and Trauma: Nerve damage resulting from accidents can interfere with the intricate coordination needed for proper urination.
- Conditions like Multiple Sclerosis: Chronic conditions affecting the nervous system can disrupt the signals essential for smooth urine flow.
3. Surgical Interventions: Unraveling Post-Operative Challenges
- Anesthesia-Induced Nerve Impairment: The aftermath of surgery can lead to nerve impairment, affecting urinary function.
- Scar Tissue Formation: Procedures on the urinary tract may contribute to scar tissue formation, constricting the urethra and causing hesitancy.
4. Infections: Probing Prostatitis and Beyond
- Prostatitis: Inflammation of the prostate gland can lead to swelling, increasing pressure on the urethra and resulting in hesitancy.
- Urinary Tract Infections (UTIs) and STIs: Infections affect both men and women, disrupting normal urine flow.
5. Shy Bladder Syndrome: Unmasking the Psychological Element
- Paruresis: Rare cases involve psychological discomfort or anxiety, particularly in public settings like bathrooms, manifesting as difficulty initiating urination.
- Social Phobia: Individuals with social phobia may experience heightened urinary hesitancy in public restrooms.
6. Medications: Unraveling Unintended Consequences
- Cold Treatments and Antidepressants: Medications can lead to altered urine habits, from reduced flow to outright hesitancy.
- Communication with Healthcare Providers: Open communication about medication side effects is crucial for managing urinary health.
7. Hormonal Influences: Exploring Imbalances
- Women and Hormonal Fluctuations: Changes during pregnancy, menopause, or conditions affecting hormonal regulation may contribute to disruptions in urinary function.
- Balancing Hormones: Hormonal imbalances need careful consideration, especially in women, for a comprehensive approach to urinary health.
Urinary Hesitancy Symptoms
Identifying the signs is paramount for recognizing urinary hesitancy:
- Difficulty initiating urination: Struggling to commence the urine stream.
- Weak or intermittent stream: A noticeable reduction in the force of urine flow.
- Incomplete emptying: The sensation of the bladder not fully emptying after urination.
- Increased urgency: Sudden, compelling needs to urinate.
When to Seek Medical Help
Recognizing emergency situations is vital, especially when coupled with urinary difficulties and clear potential urinary hesitancy causes. Red flags include vomiting, fever, shaking, chills, and low back pain, necessitating immediate medical attention.
Diagnosing Urinary Hesitancy: A Comprehensive Approach
A detailed medical history serves as the starting point for diagnosis. Essential tests, such as uroflowmetry, pressure flow testing, and video urodynamic testing, aid in identifying the root causes. For men, crucial examinations like the rectal prostate exam and imaging studies play a pivotal role.
Additional Consideration: Hormonal Influences
Hormonal imbalances, especially in women, can contribute to urinary hesitancy. Changes in hormone levels during pregnancy, menopause, or conditions affecting hormonal regulation can impact urinary function.
Urinary Hesitancy Treatment Options
Tailored approaches for lasting relief involve diverse treatments:
- Antibiotics for Infections: Addressing underlying infections.
- Medications for an Enlarged Prostate: Alleviating symptoms of BPH.
- Surgical Interventions: Relieving prostate blockage or dilating the urethra.
- Home Remedies: Complementary measures include warm baths, bladder massages, Kegel exercises, and fluid intake management.
Holistic Approach: Lifestyle Modifications
Incorporating lifestyle changes, such as maintaining a healthy weight, staying physically active, and managing stress, complements medical interventions and contributes to long-term improvements.
Patient Education: Empowering Individuals
Educating individuals about their condition fosters a proactive approach, fostering a sense of control and collaboration in the treatment journey.
Complications of Untreated Urinary Hesitancy
The repercussions of neglecting urinary hesitancy can lead to severe complications:
1. Urinary Retention
- Definition: Complete inability to empty the bladder.
- Complications: Can lead to kidney damage, urinary tract infections, and increased discomfort.
2. Surgical Considerations
- Increased Risk: Prolonged hesitancy may necessitate surgical interventions to address complications like urinary retention.
3. Impact on Quality of Life
- Psychological Strain: Long-term hesitancy may contribute to increased stress and anxiety, impacting mental well-being.
- Social Implications: Challenges in social settings, especially public restrooms, may affect an individual’s daily life.
Exploring Research Frontiers
Beyond current understanding, ongoing research aims to uncover novel insights into urinary hesitancy. Investigating potential genetic predispositions, advancements in diagnostic technologies, and emerging therapies contribute to a continuous evolution in the field.
Conclusion
Understanding urinary hesitancy is like deciphering a puzzle with many pieces. Dr. Dushyant Pawar, a best urologist expert, helps us put it all together. From the common culprit of an enlarged prostate to the psychological nuances of shy bladder syndrome, we explore the reasons behind difficulty in starting or maintaining urine flow. Dr. Pawar emphasizes the importance of seeking timely medical advice and making lifestyle adjustments for a healthier life. As we uncover more through ongoing research, this knowledge empowers you to take charge of your urinary health.
FAQs
Q: Can urinary hesitancy be treated at home?
A: Mild cases may improve with lifestyle changes, like staying hydrated, but persistent symptoms require medical attention.
Q: How is urinary hesitancy diagnosed?
A: Diagnosis involves a medical history review, physical examination, and sometimes imaging or urodynamic tests to identify the underlying cause.
Q: When should I seek medical help for urinary hesitancy?
A: Consult a healthcare professional if urinary hesitancy persists, is accompanied by pain, blood in urine, or if it significantly disrupts your daily life. Early intervention is crucial for proper management.
Q: Can urinary hesitancy affect both men and women?
A: Yes, while it is more commonly associated with men due to prostate issues, women can also experience urinary hesitancy due to factors such as pelvic floor dysfunction or urinary tract problems.
Q: Can stress or anxiety contribute to urinary hesitancy?
A: Yes, emotional factors like stress or anxiety can impact bladder function and contribute to urinary hesitancy. Managing stress through relaxation techniques may help alleviate symptoms.